Background: The prognostic significance of the difference between poststress and at rest left ventricular ejection fraction (ΔLVEF) in patients sent for di- agnostic myocardial perfusion study (MPS) is not well characterized. The purpose of this study was to prospectively evaluate the ability of ΔLVEF in further risk stratifying these patients in addition to the severity/extent of myocardial perfusion abnormalities expressed as the total perfusion deficit at stress (sTPD), according to the type of stress used.
Methods and Results: Two-day 99mTc-MIBI MPS after stress and rest were obtained for 507 patients subdivided according to the type of stress used, sTPD values, and ΔLVEF. Subsequent cardiac events were determined through a standardized questionnaire applied 1, 2, and 6 years after MPS. Independent of the type of stress used, the 6-year event rate with progressive perfusion and functional abnormalities combined was significant for total events, all-cause death, cardiac death, and revascularization but not for myocardial infarct. When ΔLVEF decreased by more than – 10%, only those individuals with sTPD of 5% or less had increased 6-year total event rates [5.9% vs 15% for those submitted to treadmill test (P < 0.001) and 8.3% vs 19% when submitted to pharmacological stress (P = 0.001)]. An sTPD greater than 5% was the only variable predictive of total events when multivariate analysis was applied (P < 0.001 for treadmill exercise and P = 0.033 for dipyridamole). Conclusions: Estimation of ΔLVEF in addition to sTPD seems to improve risk stratification for future events when ΔLVEF decreases by more than – 10% for those individuals with normal or near-normal myocardial perfusion (sTPD <= 5%). An sTPD greater than 5% was a better prognostic indicator of future events when compared with ΔLVEF for individuals with greater perfusion abnormality at stress.
Key Words: ejection fraction, myocardial perfusion, technetium, risk stratification, TPD, prognosis
(Clin Nucl Med 2012;37: 748Y754)
The simultaneous acquisition of myocardial perfusion and left ven- tricular functional data using gated SPECT (GSPECT) has led to
a significant improvement in the diagnostic accuracy for coronary artery disease (CAD) detection, with a resulting improvement in reader confidence.1-3 Furthermore, the quantification of multiple perfusion and functional parameters such as the summed scores,4 total perfusion deficit (TPD),5-8 and left ventricular ejection fraction (LVEF)9 resulted in the definitive acceptance of this imaging technique as a tool for risk stratification and the estimation of incremental prognostic
value and the impact of treatment selection on the survival analysis of CAD patients.10-21
Publications addressing these issues have focused mainly on the estimation of outcome based on the severity and extent of stress- induced perfusion abnormalities and ventricular functional data, which usually include the establishment of cutoff values for abnormal posts- tress global LVEF.10-21 Although the position statement of the Amer- ican Society of Nuclear Cardiology on the use of ECG-GSPECT22 allows for a choice between GSPECT acquisitions at rest or after stress and the consensus statement on reporting of radionuclide myocardial perfusion imaging studies23 also indicates that the assessment of left ventricular function should be performed with stress and/or rest gated techniques, there is conflicting evidence that both poststress and rest LVEF should be determined for every patient. Johnson et al24 have demonstrated that ECG-gated data acquired early after stress and at rest may represent a different physiological state, suggesting that poststress functional evaluation may not always reflect true resting measurements and that the full scope of valuable clinical information is achieved by analyzing both poststress and rest global ventricular function. On the other hand, Ramakrishna et al25 have suggested that, for most patients, poststress LVEF is an accurate reflection of rest LVEF.
Ideally, stress LVEF should be determined during stress or immediately thereafter to obtain the real-time effects of myocardial straining on regional and global myocardial function. However, bio- distribution characteristics of myocardial radiotracers such as 99mTc- MIBI allow for data acquisition between 15 and 60 minutes after tracer injection.26,27 This temporal constraint for the evaluation of stress- induced LVEF is partially overcome by the fact that regional wall motion abnormalities may persist for up to 2 hours after completion of exercise stress28 or dipyridamole testing,29 when there is postis- chemic myocardial stunning/hibernation in the absence of necrosis30 or in the presence of myocardial infarct with or without ischemia.31
Considering that same-day 99mTc-MIBI or dual-isotope myo- cardial perfusion-function study protocols have to deal with variables such as differences in tracer dose, energy, and reconstruction algo- rithms and that, at present and to our knowledge, there are no available data on the prospective prognostic evaluation of ΔLVEF for the 2-day
99mTc-MIBI imaging protocol, the purpose of this investigation was to evaluate the clinical significance of the difference between poststress and rest LVEF compared with the extent and the severity of myocar- dial perfusion abnormalities expressed by the stress TPD (sTPD) and to risk stratify patients based on ΔLVEF and according to the type of stress used.
PATIENTS AND METHODS
Study Population
This study prospectively collected perfusion and functional MPS data of 839 individuals (344 men and 495 women), sequentially sent for diagnostic MPS between May 2000 and April 2001.
Informed consent was given for answering a standardized questionnaire at 1, 2, and 6 years after the scintigraphic study, with
approval of the institution’s ethics committee. Only 507 patients completed the protocol (Fig. 1), having responded to the sixth-year questionnaire and having technically adequate MPS studies. The re- maining 332 patients were excluded owing to the lack of response to the sixth-year questionnaire (n = 304), impinging extracardiac radiotracer activity (n = 13), use of a dobutamine protocol (n = 6) and artifacts generated by arrhythmia, noncorrectable patient motion or inadequate left ventricle contouring (n = 9). Demographic, clinical characteristics, and MPS results of the included/excluded patients are described in Table 1.
Clinical Questionnaire, Endpoints, and Patient Follow-up
A standardized questionnaire was completed for every patient included in the study, containing information about the clinical status of the patient (symptoms, medication in use, and ability to perform routine tasks) and about the occurrence of hard/soft cardiac events (cardiac death, myocardial infarct, and late revascularizationVpercutaneous transluminal coronary angiography and/or coronary artery bypass graft 9 60 days after MPS) and death of any cause. Questionnaires were completed through a telephone interview performed by a researcher blinded to patient MPS data or by mail to those patients not responding. The cause of death was determined by the review of death certificates, the patient’s hospital records, and information from close relatives.
Stress Myocardial Perfusion Protocol
Patients were routinely instructed to refrain from consuming food and drugs containing methylxanthines for at least 24 hours. If possible, A-blockers were discontinued for 24 hours before MPS. A symptom-limited or an 85% maximal-load treadmill exercise test was following using the Bruce protocol. For patients unable to walk or on β-blockers, 0.56 mg of dipyridamole per kilogram of body weight [supine or walking on the treadmill with low-level exercise (LLE)] was used as a pharmacological stressor. 99mTc-MIBI (Lan-
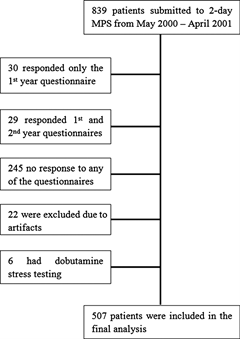
TABLE 1. Comparison of Demographic, Clinical Characteristics, and Scintigraphic Data of Patients Submitted to MPS From 2000 to 2001 According to Inclusion/Exclusion Criteria
| Included Patients | Excluded Patients | ||
| (n = 507) | (n = 332) | P | |
| Age, mean (SD), y | 59.8 (10.9) | 60.1 (11.1) | NS |
| Male, % | 40.1 | 42.4 | NS |
| BMI, mean (SD), kg/m2 | 27.3 (4.4) | 27.5 (4.9) | NS |
| Pharmacological stress, % | 44 | 54.9 | 0.002 |
| Revascularization, % | 5.7 | 5.8 | NS |
| Previous MI, % | 7.9 | 9.1 | NS |
| Diabetes, % | 12.6 | 20.9 | 0.001 |
| Hypertension, % | 61.1 | 65.5 | NS |
| Hypercholesterolemia, % | 36.5 | 43 | NS |
| Angina, % | 33 | 36.3 | NS |
| Normal MPS, % | 42.2 | 35.5 | 0.05 |
| SSS, mean (SD) | 5.3 (7.1) | 7.7 (9.9) | G0.001 |
| Rest LVEF, mean (SD), % | 61.6 (12.6) | 59.3 (16.3) | NS |
| Stress LVEF, mean (SD), % | 60.9 (13.5) | 57.9 (16.6) | NS |
theus Medical Imaging, Inc, Billerica, Mass) was injected intrave- nously with an average dose of 925 MBq (25 mCi) at the maximum treadmill workload, which was kept at that level for at least 2 minutes. For pharmacological testing, the radiotracer was injected at 4 minutes after termination of IV infusion of dipyridamole. When feasible, patients with LBBB as demonstrated in their resting ECG obtained approval from their primary physicians for the use of the vasodilator pharmacological testing protocol, when requested otherwise. End points of exercise stress were severe angina, physical exhaustion, dyspnea, sustained tachyarrhythmia, exertional hypotension, or is- chemic ST-T segment depression of at least 0.2 mV and duration of 80 milliseconds. Exercise was considered inadequate if the achieved workload was less than 80% of the predicted maximal heart rate for the particular patient, in the absence of angina or ECG is- chemic changes. Result from the dipyridamole vasodilatation stress test in the supine position was considered positive for ischemia if there is occurrence of horizontal or down-sloping ST-segment de- pression of 1 mm or greater.
GSPECT Data Acquisition and Reconstruction Protocols
All patients were submitted to a 2-day imaging protocol32 using rest-stress or stress-rest IV injection of 740 to 1295 MBq of 99mTc- MIBI based on their weight. All image acquisitions were obtained approximately 60 minutes after injection. GSPECT acquisition was obtained for rest and stress studies using a 90-degree dual-detector gamma camera (Vertex Plus ADAC Laboratories, Milpitas, Calif ). A total of 32 frames of 30-second duration using a 64 x 64 x 16-pixel matrix (pixel size, 6.33 mm) were obtained with a noncircular orbit for 180 degrees using high-resolution collimators. No attenuation or scatter correction was applied. Standard filtered backprojection was applied for image reconstruction without attenuation or scatter cor- rection. Eight bins per cardiac cycle (100% acceptance window) were obtained for determination of the functional ventricular data33 using the Cedars-Sinai’s software AutoQUANT V. 5.1.1. All studies were reprocessed by 2 of the authors (P.A.C. and P.M.A.) with the updated version AutoQUANT 6.5 for a complete final reading and non- attenuation-corrected TPD determination.
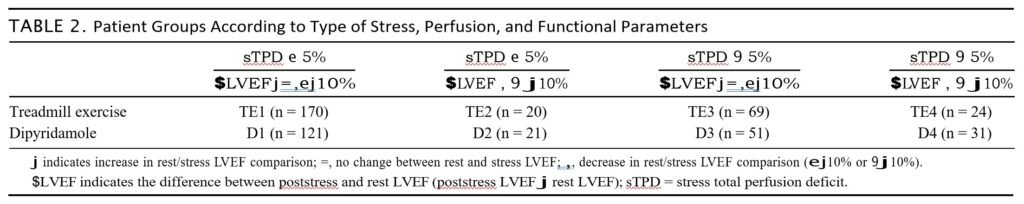
Image Interpretation and Scintigraphic Indices
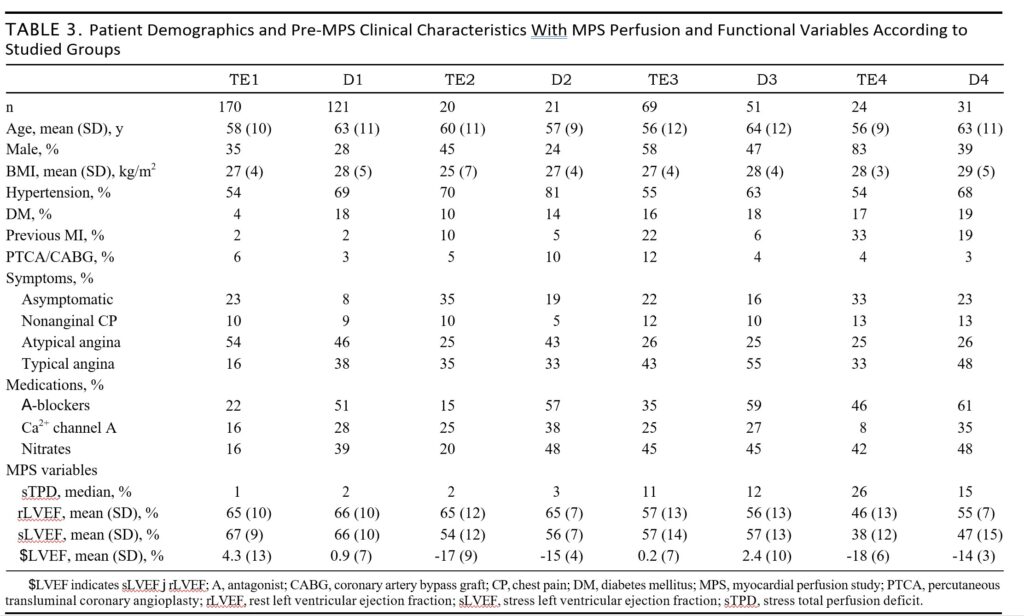
Visual interpretation of MPS images was based on short-axis and vertical and horizontal long-axis tomograms. Semiquantitative analysis was obtained with short-axis and vertical long-axis tomo- grams divided according to the 17-segment model. Summed scores, the extent of perfusion abnormalities, TPD, LVEF, and other func- tional parameters were determined automatically, without operator interference5-8,33,34 [patients with extracardiac activity within the FOV (n = 117), correctable motion during data acquisition (n = 139) were reviewed, confirming noninterference with automatic ventric- ular wall edge detection]. Patients were subdivided into 8 groups according to the type of stress used (treadmill exercise vs dipyr- idamole with or without low-level exercise), quantitative myocardial perfusion (normal/near-normal or abnormal myocardial according to sTPD <= 5% or > 5%), and ΔLVEF (difference between poststress LVEF and rest LVEF <= -10% or > -10%; Table 2). The demographic and clinical characteristics of patients included in each group are described in Table 3, along with MPS perfusion and functional data.
Patients with ischemia with ΔTPD greater than 2% (poststress TPD – TPD at rest) were compared with nonischemic individuals ($TPD <= 2%). When TPD at rest was greater than poststress TPD, ΔTPD was considered = 0.
Statistical Analysis
Continuous variables are expressed as mean (SD), unless in- dicated otherwise, as evaluated with Student t test. Statistical differ- ences between categorical variables were analyzed with X2 test for heterogeneity, and linear-by-linear association with incidence rate was calculated with simple and multiple Poisson regression with robust variances for 95% confidence intervals (CIs). P < 0.05 was considered significant. Relative risk (RR) was estimated in relation to the lowest- risk groups (T1 and D1) with a 95% CI (lower interval value >= 1.0 being considered statistically significant). Bonferroni adjustment was applied for the analysis performed (4 patient groups and 5 outcomes), with P <= 0.0025 considered significant. All analyses were conducted using SPSS/PASW Version 18.0 (IBM, Somers, NY).
RESULTS
Analysis of Event Rates and RR in the Studied Population
Sequential Analysis of sTPD and $LVEF According to the Type of Stress Used
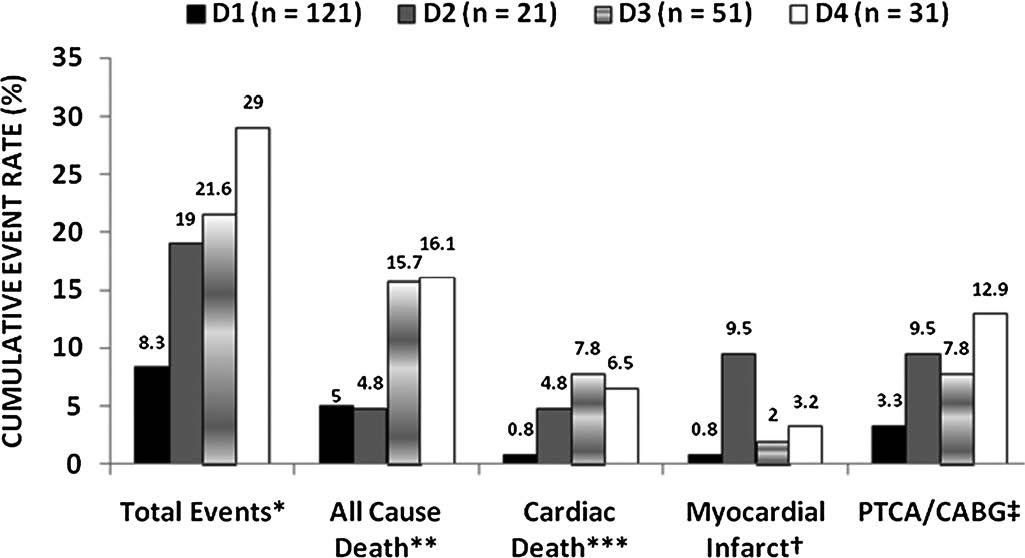
Figures 2 and 3 demonstrate that individuals with less promi- nent perfusion abnormalities (sTPD <= 5%) had increased 6-year total event rates when ΔLVEF decreased more than – 10% [5.9% vs 15% for those submitted to treadmill test (P < 0.001) and 8.3% vs 19% when submitted to pharmacological stress (P = 0.001)]. Representing 8.1% of the whole patient cohort (41/507), 76% of these individuals who presented with less perfusion abnormality and increased func- tional compromise induced by stress did not have a history of previous myocardial infarct and/or revascularization (29/41).
The 6-year event rate with perfusion and functional abnor- malities combined was significant for the total events independent of the type of stress applied (P <= 0.001) and for all cause death and revascularization but only for those individuals submitted to treadmill testing (P <= 0.001). No significant difference was observed for out- comes such as cardiac death or infarct probably because of the rela- tively small size of the sample population. Little difference in total event rate was verified in those patients with an sTPD greater than 5% when correlated to ΔLVEF. Figure 2 demonstrates that there was an actual reduction in the total event rate with ΔLVEF greater than – 10% in patients submitted to treadmill exercise, probably because of the elevated incidence of revascularization for those individuals with better global left ventricular function (ΔLVEF < – 10%).
When compared with the lowest-risk individuals in groups TE1 and D1, there was an increased RR of events for all other groups, independent of the type of stress applied (Figs. 4 and 5). Confidence intervals, however, demonstrated statistical significance mostly when there was abnormal myocardial perfusion (sTPD > 5%). For those individuals with normal or near-normal perfusion with a greater than – 10% decrease in ΔLVEF (groups TE2 and D2), there was a tendency for a significant increase in the RR for total events, with statistical significance only for the occurrence of myocardial infarct in those submitted to pharmacological stress (Fig. 5).
Analysis of ΔLVEF Independent of sTPD and According to the Type of Stress Used
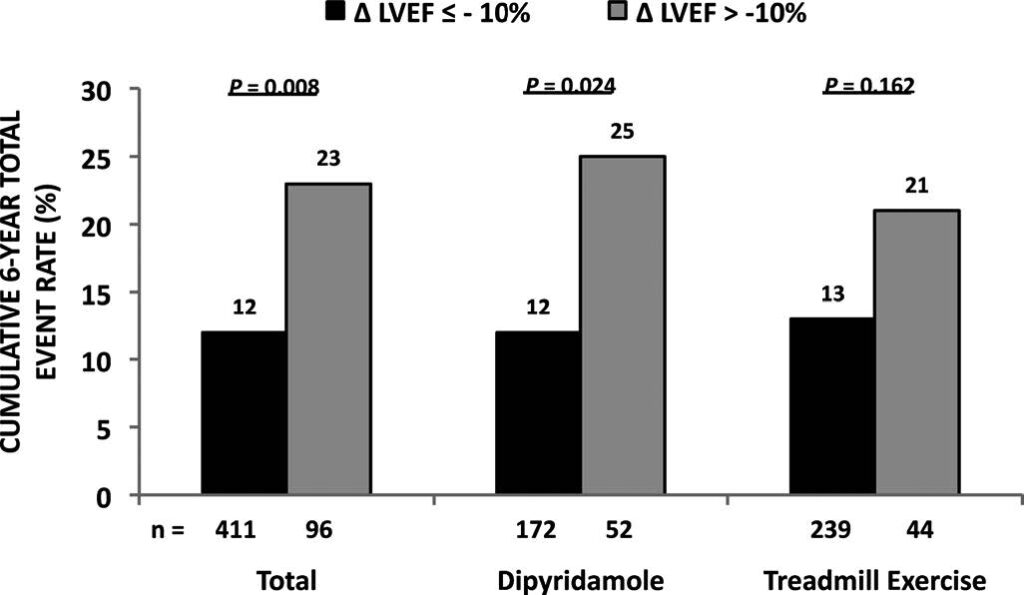
When comparing groups D1 + D3 (ΔLVEF ↑ = ↓ <= -10%, n = 172) versus D2 + D4 (ΔLVEF ↓ > -10%, n = 52), the 6-year cu-

mulative total event rate was 12.2% and 25%, respectively (P = 0.025) with an RR of 2.0 (CI, 1.1Y3.8). The comparison of groups TE1 + TE3 (ΔLVEF ↑ = ↓ < -10%, n = 239) versus TE2 + TE4 (ΔLVEF , ↓ > -10%, n = 44) demonstrated a 6-year cumulative total event rate of 12.6% and 20.5%, respectively (P = 0.163) with an RR of 1.6 (CI, 0.8 – 3.2; Fig. 6).
Analysis of ΔLVEF Independent of sTPD or the Type of Stress Used
Independent of the stress type or the presence of perfusion abnormalities, there was a significant difference when comparing those individuals with a greater than -10% decrease in ΔLVEF (n = 96) as opposed to those with an ΔLVEF -10% or less (n = 411), with a 6-year cumulative total event rate of 22.9% and 12.4%, respectively (P = 0.008) with an RR of 1.85 (CI, 1.2 – 2.9) (Fig. 6).
Analysis of sTPD Independent of ΔLVEF or the Type of Stress Used
Individuals with an sTPD greater than 5% (n = 175) com- pared with those with an sTPD of 5% or less (n = 332) had a 26.3% total event rate in 6 years as opposed to 8.1% for the group with a lower perfusion abnormality burden (P < 0.001), with an RR of 3.2 (CI, 2.1 – 5.0).

submitted to treadmill test and according to sTPD and $LVEF
combinations detailed in Table 2).

submitted to pharmacological test with dipyridamole and
according to sTPD and $LVEF combinations detailed in Table 2).
MI indicates myocardial infarct.
Sequential Analysis of $LVEF and sTPD for Individuals Submitted to Pharmacological Stress
Figure 7 demonstrates a significant difference (P = 0.019) in the 6-year cumulative total event rate between patients submitted to dipyridamole only (n = 142) versus dipyridamole associated with LLE (n = 82), with a rate of 20.4% and 6.1%, respectively, and an RR of 2.98 (CI, 1.19 – 7.45).
Comparison With Other Perfusion and Functional Variables for the Prediction of Total Events
When using a multivariate analysis of variables that included sTPD greater than 5%, a relative decrease greater than -10% in ΔLVEF, poststress LVEF less than 45%, and transient ischemic dilation (TID) of 1.2 or higher for the prediction of total events according to the typeof stress used (Table 4), an sTPDgreater than5% was the only significant predictor of total events, independent of the type of stress used (P < 0.001 for treadmill exercise and P = 0.033 for pharmacological testing with dipyridamole).
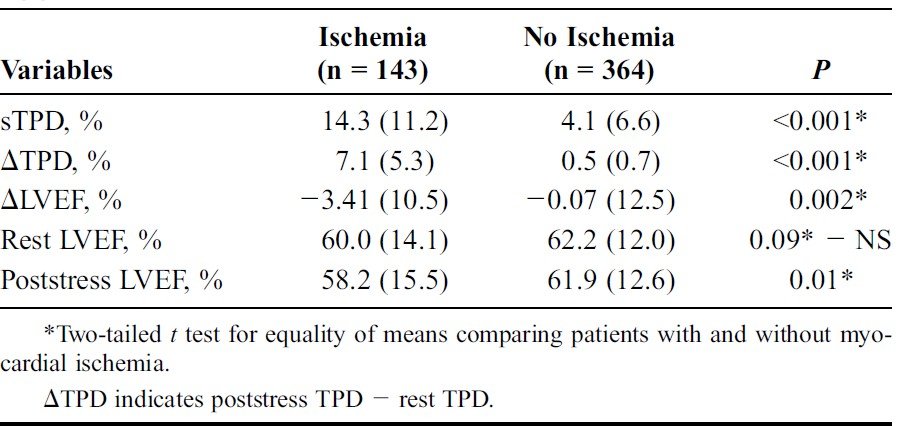
Perfusion and Functional Parameters Analyzed in Patients With Versus Without Ischemia
Table 5 summarizes the perfusion and functional parameters in patients with ischemia (ΔTPD >= 2) compared with nonischemic individuals. ΔTPD showed a significant correlation with the summed difference score for
ΔLVEF (<= -10% or > -10%) in all patients and according to the
type of stress used.

individuals submitted to dipyridamole associated with LLE or
dipyridamole only (supine at rest) according to the degree of left
ventricular perfusion and function abnormalities. n = number
of patients per group. *RR = 2.98 (1.19 – 7.45), P = 0.019.
the analyzed cohort as awhole (n = 507, r = 0.895, P < 0.001). ΔLVEF was significantly lower in patients with stressinduced ischemia (-3.41% [10.5%] vs -0.07% [12.5%], P = 0.002). Mean poststress LVEF in patients with ischemia was 58.2% (15.3%) versus 61.9% (12.6%) in those without (P = 0.01), although there was no significant difference between patients with/without ischemia for rest LVEF (P = 0.09).
DISCUSSION
The need to evaluate both poststress and rest LVEF has been deemed necessary in specific situations such as in patients with previous myocardial infarct,31 for better identification of multivessel CAD with exercise 35 or after adenosine triphosphate loading,36 and in predicting significant CAD in patients submitted to dipyridamole stress.37,38 These studies, however, have all analyzed the difference between poststress and rest LVEF from a diagnostic perspective. There is a paucity of publications addressing the prognostic impact of ΔLVEF compared with myocardial perfusion and the type of stress used in MPS. The present study suggests that the use ΔLVEF may have a broader significance in identifying individuals at a greater risk for cardiac events or death of any cause. Although hindered by a reduced

Variables in Predicting total Cumulative 6-Year Events According
to the Type of Stress Used
and Without Ischemia, Independent of the Type of Stress
Applied
number of patients caused by the subdivision of the studied cohort according to the type of stress applied, when ΔLVEF was used sequentially after the estimation of the extent and severity of perfusion abnormality at stress expressed by sTPD, individuals with a lower perfusion abnormality burden (sTPD <= 5%) were at a greater risk for events when ΔLVEF decreased by more than j10%, independent of the type of stress applied. Although not quite reaching statistical significance for the RR, probably because of the limited population sampled, it is relevant to be able to further risk stratify patients with a lower sTPD using ΔLVEF as an adjunct. When analyzing the 6-year event rate according to the type of stress used, there was no significant difference between the groups submitted to dipyridamole or treadmill testing as a whole. However, when ΔLVEF fell by more than -10%, patients submitted to pharmacological stress had a greater incidence of events when compared with those individuals submitted to dipyridamole + LLE or treadmill testing. This finding would go against the expected lower incidence of ventricular function abnormalities produced by vasodilator stress as opposed to exercise. Because little has been published regarding the added prognostic value of function measurements from 2-day GSPECT with the proposed image acquisition protocol, the present findings would point to the contrary, in agreement with the worse overall clinical status of the population usually submitted to pharmacological stressing.
As expected, individuals with an sTPD greater than 5% were also at a greater risk of events, but when an sTPD greater than 5% was compared with ΔLVEF, LVEF less than 45%, and TID of 1.2 or higher using multivariate analysis, only a sTPD greater than 5% was predictive of total cumulative 6-year events (P < 0.001 for treadmill exercise and P = 0.033 for dipyridamole). This would imply a relatively greater importance of stress perfusion abnormalities than the actual changes in global poststress/rest LVEF for those individuals with greater perfusion abnormality (sTPD > 5%). However, it is possible that, for this particular patient cohort sent primarily for diagnostic MPS with a low prevalence of CAD and normal average LVEF, less functional impairment of the left ventricle or the temporal constraint
imposed by the used imaging protocol inducing a physiological shift toward normal global left ventricular function may be a factor collaborating with the underestimation of the prognostic capability of ΔLVEF. It is felt, however, that this finding does not invalidate the fact that patients with a lower perfusion abnormality burden at stress when presenting a greater than 10% decrease of ΔLVEF may need a more rigorous and aggressive follow-up owing to the suggested increase in the total 6-year event rate. Because only 8% of the studied patient cohort presented with normal/near-normal perfusion accompanied by a significant decrease in ΔLVEF, future studies will be paramount for the evaluation of the prognostic impact of ΔLVEF determination in the setting of diagnostic MPS for CAD.
LIMITATIONS
The significant loss of patient follow-up (39.57% of the initial database) is certainly a factor that influenced the obtained results, especially considering that the excluded individuals were ‘‘sicker’
patients. Furthermore, subgrouping of the patient database induced a significant reduction in the number of individuals that constituted each of the different groups when analyzing stress modality, perfusion, and functional characteristics, reducing the statistical power of the analysis. Therefore, other studies are necessary to corroborate the presented results.
Because the acquired MPS were nonYattenuation corrected, a slightly higher value for sTPD cutoff was applied in an attempt to reduce eventual false-positive perfusion abnormalities. A correlation of the present findings with state-of-the-art technology such as a combined quantitative analysis of attenuation-corrected and noncorrected myocardial perfusion SPECT is warranted.
Other potential confounding factors include the fact that small ventricles were not excluded and that other parameters that may influence LVEF determination, such as loading ventricular conditions (blood pressure and heart rate), were not controlled. It should be emphasized that the present results pertain only to the 2-day 99mTc- MIBI GSPECT protocol with a 1-hour interval between stress/rest and imaging. Although applied in many laboratories, protocols with this timing constraint may induce a selection bias with patients having eventual functional abnormalities improved before imaging was performed.
CONCLUSIONS
The estimation of ΔLVEF in addition to sTPD showed a tendency toward improving risk stratification for future events when ΔLVEF decreased by more than -10% for those individuals with normal or near-normal myocardial perfusion (sTPD <= 5%). An sTPD greater than 5% was a better prognostic indicator of future events when compared with ΔLVEF for those individuals with greater perfusion abnormality. Patients submitted to pharmacological stress with supine dipyridamole were at a higher risk when compared with their counterparts submitted to dipyridamole with LLE.
ACKNOWLEDGMENTS
The authors thank Daniel Lemke, BSc, and Betina B. Carvalho, BSc, for the invaluable work on data gathering.
REFERENCES
- Berman DS, Hachamovitch R, Kiat H, et al. Incremental value of prognostic testing in patients with known or suspected ischemic heart disease: a basis for optimal utilization of exercise technetium-99m sestamibi myocardial perfusion single-photon emission computed tomography. JAm Coll Cardiol. 1995; 26:639Y647.
- Smanio PE, Watson DD, Segalla DL, et al. Value of gating of technetium-99m sestamibi single-photon emission computed tomographic imaging. J Am Coll Cardiol. 1997;30:1687Y1692.
- Hachamovitch R. Clinical value of combined perfusion and function imaging in the diagnosis, prognosis, and management of patients with suspected or known coronary artery disease. In: Germano G, Berman DS, eds. Clinical Gated Cardiac SPECT. Malden, MA: Blackwell; 2006:189Y215.
- Hachamovitch R, Berman DL, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535Y543.
- Slomka PJ, Nishina H, Berman DS, et al. Automated quantification of myocardial perfusion SPECT using simplified normal limits. J Nucl Cardiol. 2005; 12:66Y77.
- Slomka PJ, Fish MB, Lorenzo S, et al. Simplified normal limits and automated quantitative assessment for attenuation-corrected myocardial perfusion SPECT. J Nucl Cardiol. 2006;13:642Y651.
- Germano G, Kavanagh PB, Slomka PJ, et al. Quantitation in gated perfusion SPECT imaging: the Cedars-Sinai approach. J Nucl Cardiol. 2007;14:433Y454.
- Berman DS, Kang X, Gransar H, et al. Quantitative assessment of myocardial perfusion abnormality on SPECT myocardial perfusion imaging is more reproducible than visual expert analysis. J Nucl Cardiol. 2009;16:45Y53.
- Germano G, Van Kriekinge S, Berman DS. Regional and global ventricular
function and volumes from SPECT perfusion imaging. In: Zaret BL, Beller GA, eds. Clinical Nuclear Cardiology. Philadelphia, PA: Mosby; 2010:194Y221. - Thomas GS, Miyamoto MI, Morello AP, et al. Technetium-99m sestamibi myocardial perfusion imaging predicts clinical outcome in the community outpatient setting. J Am Coll Cardiol. 2004;43:213Y223.
- Taillefer R, DePuey EG, Udelson JE, et al. Comparative diagnostic accuracy of Tl-201 and Tc-99m sestamibi SPECT imaging (perfusion and ECGYgated SPECT) in detecting coronary artery disease in women. J Am Coll Cardiol. 1997;29:69Y77.
- Hachamovitch R, Berman DS, Kiat H, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease: incremental prognostic value and use in risk stratification. Circulation. 1996;93:905Y914.
- Hachamovitch R, Hayes SW, Friedman JD, et al. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900Y2907.
- Shaw LJ, Berman DS, Maron DJ, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden. Results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117:1283Y1291.
- Travin MI, Heller GV, Johnson LL, et al. The prognostic value of ECGYgated SPECT imaging in patients undergoing stress Tc-99m sestamibi myocardial perfusion imaging. J Nucl Cardiol. 2004;11:253Y262.
- Sharir T, Germano G, Kavanagh PB, et al. Incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation. 1999; 100:1035Y1042.
- Sharir T, Germano G, Kang XK, et al. Prediction ofmyocardial infarction versus cardiac death by gated myocardial perfusion SPECT: risk stratification by the amount of stress-induced ischemia and poststress ejection fraction. J Nucl Med. 2001;42:831Y837.
- Hachamovitch R, Hayes SW, Friedman JD, et al. Is there a referral bias against catheterization of patients with reduced left ventricular ejection fraction? J Am Coll Cardiol. 2003;42:1286Y1294.
- Sharir T, Kang X, Germano G, et al. Prognostic value of post-stress left ventricular volume and ejection fraction by gated myocardial perfusion SPECT in women and men: gender-related differences in normal limits and outcomes. J Nucl Cardiol. 2006;13:495Y506.
- Bourque JM, Velazquez EJ, Tuttle RH, et al. Mortality risk associated with ejection fraction differs across resting nuclear perfusion findings. J Nucl Cardiol. 2007;14:165Y173.
- America YGCJ, Bax JJ, Boersma E, et al. The additive prognostic value of perfusion and functional data assessed by quantitative gated SPECT in women. J Nucl Cardiol. 2009;16:10Y19.
- Bateman TM, Berman DS, Heller GV, et al. American Society of Nuclear Cardiology position statement on electrocardiographic gating of myocardial perfusion SPECT scintigrams. J Nucl Cardiol. 1999;4:470Y471.
- Hendel RC, Wackers FJT, Berman DS, et al. American Society of Nuclear Cardiology consensus statement: reporting of radionuclide myocardial perfusion imaging studies. J Nucl Cardiol. 2006;13:e152Ye156.
- Johnson LL, Verdesca SA, AudeWY, et al. Postischemic stunning can affect left ventricular ejection fraction and regional wall motion on post-stress gated sestamibi tomograms. J Am Coll Cardiol. 1997;30:1641Y1648.
- Ramakrishna G, Miller TC, Hodge DO, et al. Differences in left ventricular ejection fraction and volumes measured at rest and poststress by gated sestamibi SPECT. J Nucl Cardiol. 2006;13:668Y674.
- Taillefer R, Lambert R, Bisson G, et al. Myocardial technetium 99m labeled sestamibi single photon emission computed tomography imaging in the detection of coronary artery disease: comparison between early (15 minutes) and delayed (60 minutes) imaging. J Nucl Cardiol. 1994;1:441Y448.
- Strauss HW, Miller DD, Wittry MD, et al. Procedure guideline for myocardial perfusion imaging 3.3. J Nucl Med Technol. 2008;36:155Y161.
- Ambrosio G, Betocchi S, Pace L, et al. Prolonged impairment of regional contractile function after resolution of exercise-induced angina: evidence of myocardial stunning in patients with coronary artery disease. Circulation. 1996;94:2455Y2464.
- Lee DS, Yeo JS, Chung JK, et al. Transient prolonged stunning induced by dipyridamole and shown on 1- and 24-hour post-stress Tc-99m MIBI gated SPECT. J Nucl Med. 2000;41:27Y35.
- Vanoverschelde JL, Wijns W, Depre C, et al. Mechanisms of chronic regional postischemic dysfunction in humans. Circulation. 1993;1513Y1523.
- Bavelaar-Croon CDL, America YGCJ, Atsma DE, et al. Comparison of left ventricular function at rest and post-stress in patients with myocardial infarction: evaluation with gated SPECT. J Nucl Cardiol. 2001;8:10Y18.
- Hayes SW, Berman DS, Germano G. Stress testing and imaging protocols. In: Germano G, Berman DS, eds. Clinical Gated Cardiac SPECT. Malden, MA: Blackwell; 2006:47Y68.
- Germano G, Kiat H, Kavanagh P, et al. Automatic quantification of ejection fraction fromgatedmyocardial perfusion SPECT.J NuclMed. 1995;36:2138Y2147.
- Xu Y, Heyes S, Ali I, et al. Automatic and visual reproducibility of perfusion and functional measures for myocardial perfusion SPECT. J Nucl Cardiol. 2010;17:1050Y1057.
- Hida S, Chikamori T, Tanaka H, et al. Diagnostic value of left ventricular function after stress and at rest in the detection of multivessel coronary artery disease as assessed by electrocardiogram-gated SPECT. J Nucl Cardiol. 2007;14:68Y74.
- Hida S, Chikamori T, Tanaka H, et al. Diagnostic value of left ventricular function after adenosine triphosphate loading and at rest in the detection of multi-vessel coronary artery disease using myocardial perfusion imaging. J Nucl Cardiol. 2009;16:20Y27.
- Hung GU, Lee KW, Chen CP, et al. Worsening of left ventricular ejection fraction induced by dipyridamole on Tl-201 gated myocardial perfusion imaging predicts significant coronary artery disease. J Nucl Cardiol. 2006; 13:225Y232.
- Wienmann P, Moretti JL. Effects of dipyridamole on left ventricular function. J Nucl Cardiol. 2000;7:103Y106.

